Abstract
Background: Signals provided by the microenvironment can modify and circumvent pathway activities that are therapeutically targeted by drugs. However, a systems-level understanding of how the microenvironment and the genetic and molecular alterations of the tumor interact with each other and contribute to drug resistance is lacking.
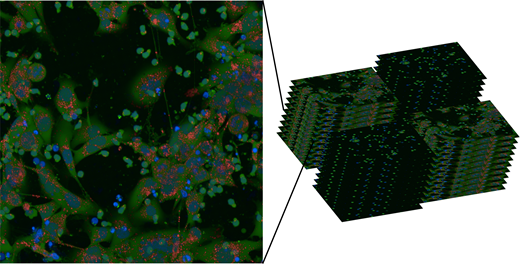
Methods: To address this unmet need, we established an automated microscopy-based phenotyping platform that uses co-culture conditions mimicking the bone marrow environment. We cultured primary tumor cells from more than 100 leukemia patients (CLL, AML, MCL, T-PLL, HCL) with and without bone marrow stroma cell support in DMEM and 10% human serum and treated each condition with 57 drugs in 3 concentrations. After 72h of incubation, 22 000 images per patient were acquired and processed by our custom made image analysis pipeline. Our set-up allows us to increase sensitivity far beyond simple viability testing, as it reads out additional cell type specific features such as cell morphology, autophagy and cell-cell interactions.
Results: Quality assessment revealed that in contrast to mono-culture conditions, assay plate edge effects can be avoided under stable stroma cell co-culture conditions. Correlation of replicated patient samples were comparable between mono- and co-cultures (R2>0.75).
In the absence of their native microenvironment, primary leukemia cells undergo spontaneous apoptosis ex-vivo. Viability at culture start was always >90% and dropped to a median of 51% (viability range: 17%-90%) after 72h in mono-cultures. Among CLL samples spontaneous apoptosis was not dependent on either IGHV mutation status or any major cytogenetic risk group. Bone marrow stroma cell co-culture conditions protected tumor cells from spontaneous apoptosis (p=8.2e-6, paired t-test). Patient samples with a high degree of spontaneous apoptosis benefited most from co-culture conditions (p=7.2e-10, Pearson correlation).
To model interactions of stroma cell conditions and drug-induced apoptosis we established the following linear model: Viability ~ drug-effect + culture-model + drug-effect:culture-model. While activity of some drugs was significantly altered under co-culture conditions, we could also identify drugs with similar activity in mono- and co-cultures. For instance, the activity of common chemotherapeutics (fludarabine: p=0.002 at 0.6µM, cytarabine: p=0.001 at 1.5µM, ANOVA) or bromodomain inhibitors (I-BET-762: p=5.9e-5 at 4.5µM, JQ1: p=1.5e-8 at 1.5µM, ANOVA) was significantly reduced under co-culture conditions. In contrast, PI3K inhibitors idelalisib and duvelisib had a similar activity in mono-culture and stroma co-culture conditions and might represent a starting point to overcome stroma cell mediated drug resistance. In CLL, we identified IGHV mutation status and trisomy 12 as important determinants of response to kinase inhibitors. We confirmed these findings in stroma cell co-cultures, e.g. a better activity of B-cell receptor inhibitors in trisomy 12 and IGHV unmutated CLL. A systematic comparison of ex-vivo drug response pattern in mono- and co-cultures across 171 drug conditions will be presented.
Conclusion: Our results suggest that high throughput co-culture drug testing can be robustly performed and provide an unprecedented understanding of how the stroma cell microenvironment and the genetic make-up of tumor cells contribute to drug resistance and sensitivity.
Figure: Over 2 million microscopy images were acquired and analysed to assess drug resistance and sensitivity in a co-culture model of primary leukemia and bone marrow stroma cells. blue= Hoechst33342, green=Calcein AM, red=lysosomal dye NIR
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal